
Medical Database & Alert System
2025
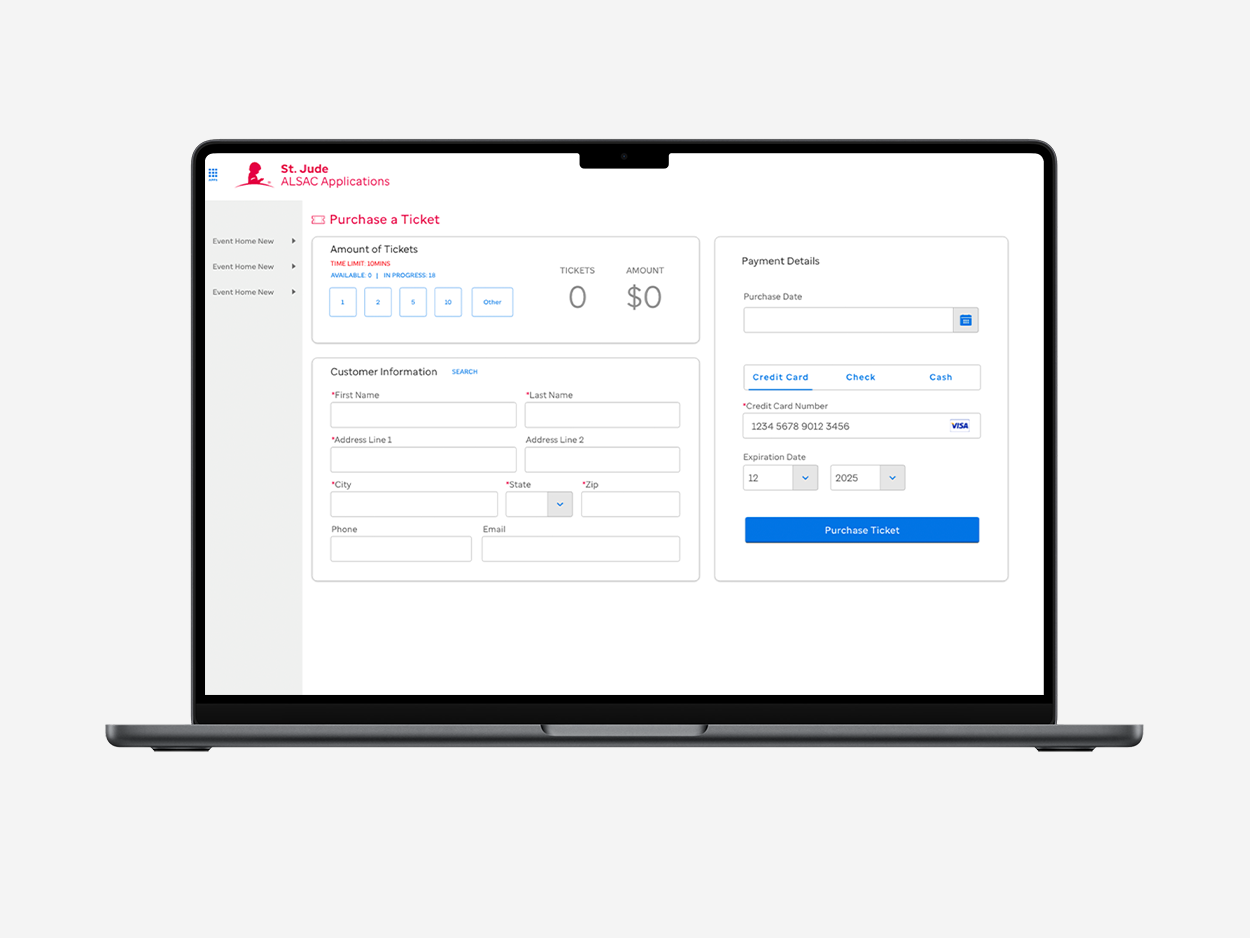
Donation Intake Form
2021

Product Visualizer
2019
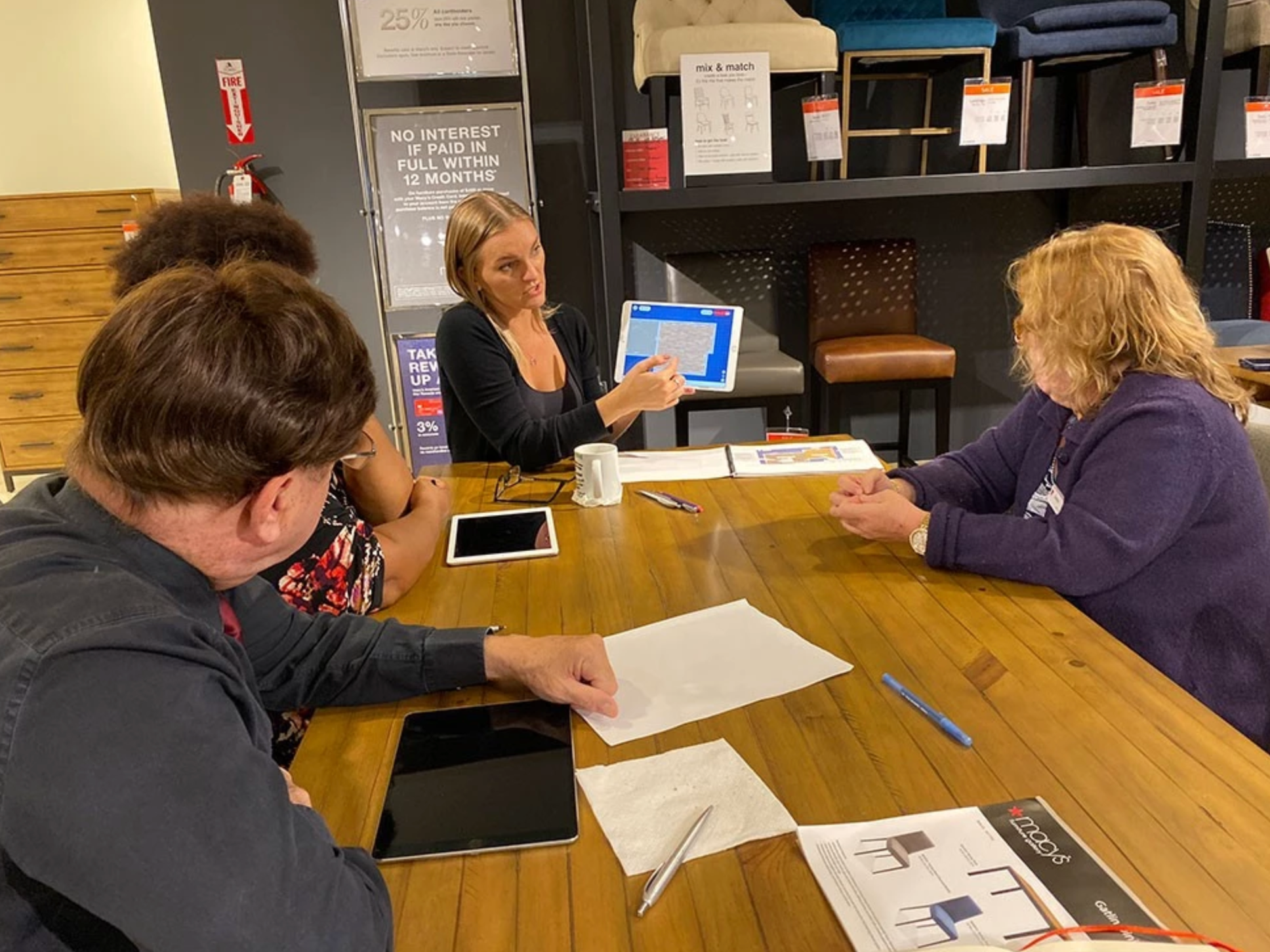
User Testing Research
2018
